Background :A panel of laboratory tests are used to diagnose iron deficiency anemia, including hemoglobin (Hb), mean cell volume (MCV), serum ferritin, total iron binding capacity (TIBC), and iron saturation (ISAT). Newer diagnostic biomarkers include reticulocyte hemoglobin (RHb). The association between these parameters and response to intravenous iron have not been well characterized. The aim of this study was to evaluate the associations between baseline laboratory values commonly used in diagnosis of iron-deficiency anemia and improvement in hemoglobin concentration (Hb).
Methods :Data was collected retrospectively using The Ottawa Hospital Data Warehouse (OHDW) reflecting practices from 3 local institutions. Patients that received at least 1 intravenous iron infusion between 2007 and 2018 were included. Patients that received intravenous iron replacement with baseline hemoglobin and at least one hemoglobin measured after the last documented iron infusion were included. Patients transfused within 90 days of the last infusion were excluded. For patients that received more than one course of iron replacement, each course was included separately if the time between the last infusion of the earlier course and the first infusion of the later course were at least 180 days apart. The primary outcome was achieving a maximum change in Hb of ≥10 g/L after the last iron infusion. Logistic regression was used to measure the association between pre-infusion laboratory characteristics (Hb, mean cell volume [MCV], platelet and reticulocyte count, reticulocyte Hb, ferritin, total iron binding capacity [TIBC], and iron saturation [ISAT]), age, sex, and presence of chronic kidney disease (CKD[serum creatinine >177 µmol/L]) and the primary outcome. A multivariable logistic regression model was used to adjust for baseline characteristics and the primary outcome, adjusting for iron replacement characteristics.
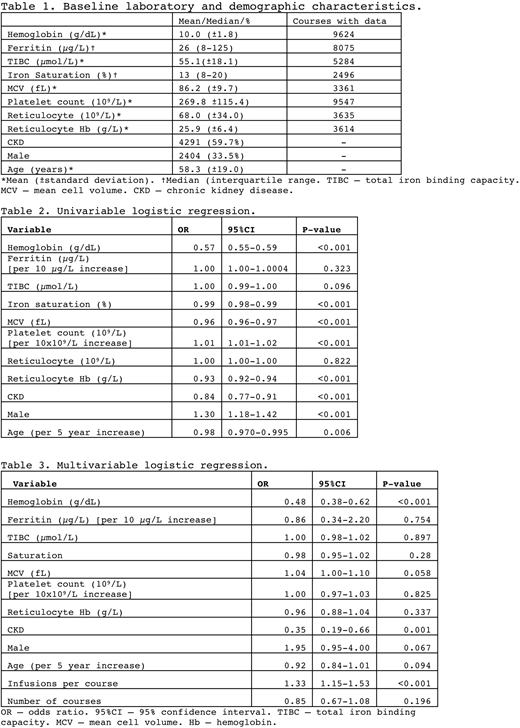
Results :Between 2007 and 2018, a total of 8326 patients were treated with intravenous iron replacement, of whom 7185 were not transfused 90 days before the last administered dose of iron. Baseline characteristics of these patients are summarized in Table 1. The median maximum post-infusion hemoglobin was 119 g/L (interquartile range [IQR] 107-30 g/L), with a median change from pre-infusion hemoglobin of 16 g/L (IQR 5-31). The maximum Hb was measured a median of 62 days (IQR 6-144 days) after the last infusion. Results of univariable (Table 2) and multivariable (Table 3) regression are shown in Tables 2 and 3, respectively. In the multivariable model, pre-infusion Hb was the only evaluated laboratory value associated with Hb response (OR 0.48 95% confidence interval (95%CI) 0.38-0.62, p<0.001). Presence of CKD (OR 0.35, 95%CI 0.19-0.66, p=0.001) and the number of infusions given per course (OR 1.33, 95%CI 1.15-1.53, p<0.001) were also associated with hematologic response.
Conclusions:In this single-center, retrospective cohort of patients treated with intravenous iron replacement and not transfused red blood cells within 90 days of the last infusion, most evaluated baseline characteristics were not associated with achieving a ≥10 g/L improvement in Hb concentration. Baseline Hb concentration was associated with Hb response, with higher baseline Hb associated with a lower probability of a 'good' Hb response. The presence of CKD was also associated with lower chance of hematologic response. The study has several important limitations including the lack of diagnostic data relating to the need for iron infusions, concomitant oral supplementation, and potential infusions outside the study site. Pre-infusion laboratory values were missing for a large proportion of patients. The strengths of the study include the large sample size and broad inclusion criteria, allowing for increased generalizability. Further exploration of serum biomarkers in the prediction of hemoglobin responses in parenteral iron supplementation is warranted in prospective studies with scheduled laboratory measurements.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal